Understanding Modern Approaches to Varicose Vein Treatment
Why Varicose Veins Matter: Context, Stakes, and What This Guide Covers
Outline of the article you’re about to read:
– Section 1: Why varicose veins matter and how treatment decisions are framed.
– Section 2: Sclerotherapy—mechanism, candidacy, outcomes, and trade-offs.
– Section 3: Laser therapy—endovenous and surface laser modalities compared.
– Section 4: Compression stockings—evidence, choosing the right pair, and adherence.
– Section 5: Putting it all together—sequencing, recovery, costs, and lifestyle.
Varicose veins aren’t just visible lines on the skin; they are a sign that the one-way valves inside your leg veins aren’t working as efficiently as they should. When those valves falter, blood can pool, venous pressure rises, and veins distend. The result ranges from cosmetic spider webs to ropey, aching veins and symptoms such as heaviness, throbbing, nighttime cramps, and swelling. Global estimates suggest that visible varicose veins affect a substantial share of adults, with prevalence commonly reported between 20% and 30%, increasing with age and influenced by genetics, hormonal shifts, pregnancy, prolonged standing, and weight.
Why this matters goes beyond appearance. Chronic venous insufficiency can impair daily comfort, reduce mobility, and, in advanced cases, contribute to skin changes like hyperpigmentation, eczema, or even ulcers near the ankles. Not everyone will progress that far, but attentive treatment can ease symptoms and, for many, prevent a slow drift toward more persistent complaints. It’s also a quality-of-life issue: when your legs feel lighter and look calmer, you may walk farther, stand a bit taller, and re-engage in activities you had begun to avoid.
Treatment is not one-size-fits-all. The “right” choice depends on vein size and location, symptoms, ultrasound findings, and personal priorities—downtime, cost, needle tolerance, and cosmetic goals. The three pillars covered here overlap but address different needs:
– Sclerotherapy targets smaller varicose veins and spider veins efficiently.
– Laser therapy can shut down larger faulty veins from the inside or tackle fine surface vessels.
– Compression stockings support circulation, often as first-line care and after procedures.
Think of modern vein care as a toolkit. No single tool does everything, but selecting the right combination can produce steady, meaningful relief. The next sections translate clinical concepts into plain language: how each option works, how it feels, typical timelines, and how to compare them without guesswork.
Sclerotherapy: A Precise Fix for Small and Medium Problem Veins
Sclerotherapy is a minimally invasive procedure that uses a liquid or foam solution—called a sclerosant—to irritate the vein lining. This irritation causes the vein walls to stick together, collapse, and eventually be reabsorbed by the body. It’s often used for spider veins and small to medium varicose veins that are visible under the skin, especially when ultrasound shows no major reflux in a larger feeding vein. Sessions are done in an office setting, typically take 20–40 minutes, and require little to no downtime beyond walking and avoiding strenuous exertion for a short period.
What does the experience feel like? Most people report mild stinging or a pressure sensation as the solution is injected through a very fine needle. Treated veins may look darker initially and then fade over weeks to months. Multiple sessions are commonly needed to address a network of vessels thoroughly; think of this like pruning a garden—methodical, targeted, and repeated for the neatest result. Wearing compression stockings for several days to two weeks afterward can improve outcomes by supporting vein closure and reducing swelling or bruising.
Effectiveness is well-documented for smaller veins. Studies report high clearance rates of spider veins and small reticular veins after a series of treatments, with patient satisfaction frequently strong when realistic goals are set. For medium veins, foam formulations are often used to increase contact with the vein wall, improving efficacy. That said, sclerotherapy is not a cure for the tendency to form varicose veins; new veins can appear over time, particularly if underlying valve issues persist or risk factors remain.
Potential side effects are typically mild but worth noting:
– Temporary bruising and redness around injection sites are common.
– Light brown hyperpigmentation along the treated vein can happen and usually fades over months.
– Matting—tiny blush-like clusters of vessels—may develop near the treatment area and can be addressed with additional sessions.
– Rare events include inflammation, small superficial clots, or allergic reactions; proper technique and screening lower these risks.
Who is a good candidate? Individuals with symptomatic or cosmetically bothersome small-to-medium veins, especially when duplex ultrasound rules out significant reflux in a major trunk vein, often do well. Those on their feet all day, postpartum individuals, or people with a family history of vein disease are frequent seekers of sclerotherapy. It’s also a strategic follow-up after closing a larger faulty vein with thermal ablation, tidying up the remaining visible branches. Costs vary by region and extent of treatment; multiple modest sessions may be more cost-effective than one large, exhaustive attempt. The value proposition is clear: targeted relief, low downtime, and steady cosmetic gains with a series-based approach.
Laser Therapy: Closing Faulty Pathways from the Inside Out (and Treating Surface Vessels)
Laser therapy in vein care comes in two flavors. The first is endovenous laser treatment, which guides a thin fiber into a larger malfunctioning vein—commonly in the thigh or calf—under ultrasound. The fiber emits controlled heat that seals the vein from the inside, rerouting blood into healthier pathways. The second is surface laser treatment, used for fine spider veins and small red or blue vessels close to the skin. While the word “laser” sounds dramatic, these techniques are thoughtfully calibrated and have become a cornerstone of contemporary venous care.
Endovenous laser treatment (often abbreviated EVLT or EVLA) addresses the root cause when ultrasound confirms reflux in a major superficial vein. Local anesthesia and tumescent fluid around the vein protect surrounding tissues and enhance comfort. Most people walk immediately after the procedure, and typical activity restrictions are modest for a few days. Published closure rates for appropriate candidates are high at one year, commonly reported in the 90–98% range, with low recurrence when paired with lifestyle support and, if needed, adjunctive treatments like sclerotherapy for residual surface veins.
Surface laser treatment targets tiny vessels that are difficult to inject or that didn’t respond fully to sclerotherapy. It uses brief pulses of light tuned to hemoglobin to heat and collapse those vessels. Multiple sessions are the norm, spaced weeks apart. People with lighter skin tones tend to have more predictable outcomes, but thoughtful settings and test spots can expand applicability. Temporary redness, mild swelling, and a sunburn-like sensation are common, usually resolving within days. Sun protection is essential before and after to reduce pigment changes.
How does laser compare to other choices?
– Versus sclerotherapy: Lasers shine for very fine or red facial-like vessels on the legs and for closing large refluxing veins from the inside; sclerotherapy is often more efficient for blue reticular networks and many spider veins on the limbs.
– Versus surgical stripping: Endovenous laser has largely replaced older surgical approaches for many patients, offering smaller incisions, quicker recovery, and office-based convenience.
– Versus watchful waiting: In symptomatic reflux, treating the primary faulty vein often provides more than cosmetic relief—many report lighter legs, reduced swelling, and fewer cramps.
Risks are uncommon but deserve attention. For endovenous laser, mild bruising, a tugging sensation along the treated pathway, and transient numbness can occur. The chance of deep vein thrombosis is low with modern protocols that emphasize walking, hydration, and compression. Surface laser complications include blistering or pigment changes if settings are too aggressive or after sun exposure; careful technique and post-care reduce these risks. For many, the combination strategy—close the main leaky vein with laser, refine residual surface veins with sclerotherapy or additional laser—delivers durable, well-regarded results with minimal disruption to daily life.
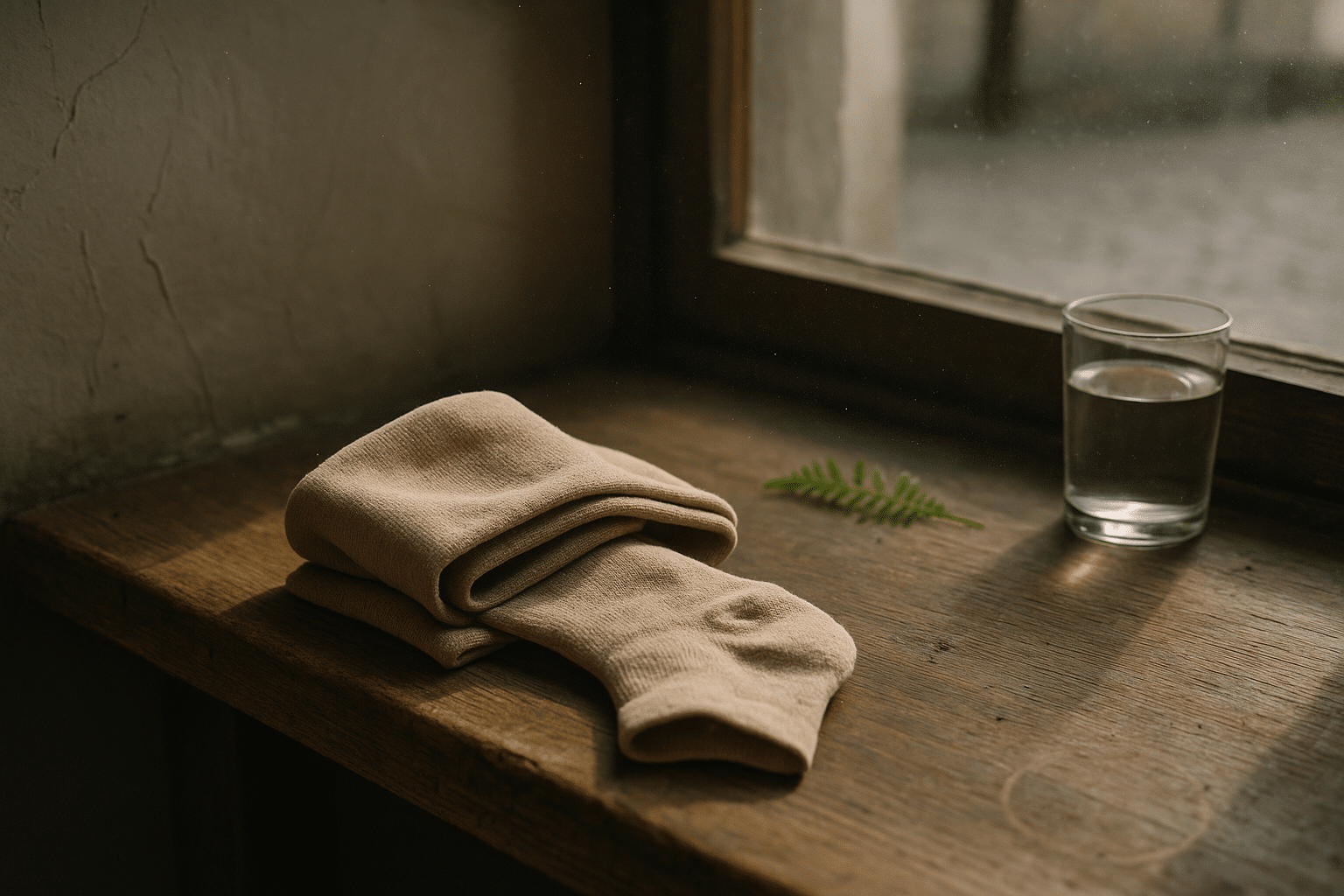
Compression Stockings: Everyday Support with Evidence and Practical Limits
Compression stockings are the quiet workhorses of vein care. By applying graduated pressure—snugger at the ankle, decreasing up the leg—they help squeeze blood upward, reducing pooling and easing symptoms like heaviness, swelling, and fatigue. They are used alone for conservative management, to stabilize symptoms during pregnancy or prolonged standing, and as an adjunct after procedures such as sclerotherapy or endovenous laser. The evidence base supports meaningful symptom relief and improved function for many users, particularly when worn consistently during waking hours.
Choosing the right pair requires attention to details:
– Compression strength: Common ranges are 15–20 mmHg (light), 20–30 mmHg (moderate), and 30–40 mmHg (firm). Many start at moderate for symptomatic varicose veins, stepping up or down under clinical guidance.
– Length: Knee-highs often suffice for calf-dominant symptoms; thigh-high or pantyhose styles may be considered if swelling or varicosities extend above the knee.
– Fit: Accurate measurements first thing in the morning—ankle, calf, and sometimes thigh circumference and leg length—help avoid slippage and discomfort.
– Material: Breathable weaves or softer knits can improve day-long wearability, and open-toe designs can reduce toe crowding.
Adherence is the linchpin. Even well-chosen stockings deliver little benefit if they stay in the drawer. Tips that make them part of real life include putting them on before getting out of bed or after elevating the legs for a few minutes, using donning gloves or a slip sock to ease the fabric up, and washing them regularly to restore elasticity. Expect to replace pairs every few months of regular use, as stretch fatigues and effectiveness wanes.
What do stockings not do? They don’t eliminate veins; they manage symptoms and can slow progression for some. For people with significant reflux in a large superficial vein, stockings may provide relief but won’t usually resolve the underlying valve failure. Side effects are uncommon and mostly practical: warmth in hot weather, marks on the skin at the band, or itching if the fabric is too coarse or dry skin isn’t moisturized. People with advanced arterial disease, certain neuropathies, or skin conditions should be screened before using higher-pressure garments.
From a cost and convenience perspective, compression is often the most accessible starting point. It’s also valuable after procedures, improving comfort and, in many protocols, supporting better early outcomes. Viewed as part of a layered strategy—daily support now, definitive intervention when indicated—compression stockings earn their place as a reliable, well-regarded foundation of care.
Choosing Your Path: Comparing Options, Sequencing Care, and Long-Term Habits
Finding the right approach is a matter of matching goals with anatomy, time, and tolerance. A practical way to think about it is in three steps: confirm the map, pick the tool, and plan the follow-through. Confirming the map means getting a focused evaluation that may include duplex ultrasound. This identifies whether a major superficial vein has reflux (often requiring endovenous treatment) or whether the problem is primarily small surface veins (more suited to sclerotherapy or surface laser). With the map in hand, choices become clearer, timelines feel less mysterious, and expectations align with reality.
How the options stack up for common scenarios:
– Cosmetic spider veins with minimal symptoms: Sclerotherapy is often efficient; surface laser can help red, fine vessels or areas not easily injected.
– Small-to-medium clusters with mild ache: Sclerotherapy remains a versatile first move, sometimes paired with light compression afterward.
– Documented reflux in a larger vein with heaviness or swelling: Endovenous laser is a widely adopted solution to shut down the faulty pathway, followed by sclerotherapy to tidy the surface network.
– Pregnancy-related symptoms: Compression stockings are a conservative mainstay; procedural treatments typically wait until after delivery and nursing unless special circumstances arise.
Recovery and expectations:
– Sclerotherapy: Walk the same day, avoid high-intensity workouts for a short window, wear compression as recommended, and expect visible fading over weeks to months. Multiple sessions fine-tune results.
– Endovenous laser: Return to daily walking immediately, brief tenderness or a pulling sensation along the treated track is normal, and compression is often advised for one to two weeks. Leg lightness and swelling improvement can be felt quickly for many.
– Surface laser: Mild redness or warmth for a day or two, with incremental fading after a series.
Costs and practicalities vary by region, insurance coverage, and the number of sessions. A straightforward sclerotherapy plan may be the most economical for small networks, while a refluxing main vein typically requires a one-time endovenous procedure plus selective touch-ups. Whichever route you choose, long-term habits amplify your investment: walking, calf raises during desk time, periodic leg elevation, weight management, and smart breaks from prolonged sitting or standing. Hydration and skin care matter too; healthy skin tolerates compression and post-procedure care more comfortably.
Ultimately, think of vein treatment as a journey, not a single mile marker. The first step—getting a clear diagnosis and understanding your options—sets the tone. Then, choose one of the top options for your situation, commit to the plan, and pair it with everyday habits that keep blood moving in the right direction. With thoughtful sequencing and realistic goals, many people find that their legs feel lighter, look calmer, and carry them through the day with renewed ease.