Understanding the Process and Benefits of Dental Implants
Outline:
– Introduction: Why implants are a modern cornerstone in dentistry
– The oral surgery journey: assessment, planning, placement, healing
– Prosthetic choices: crowns, bridges, overdentures, materials
– Outcomes, risks, maintenance, and lifestyle considerations
– Conclusion and practical next steps for patients
Dentistry Today: Why Implants Matter and Where They Fit
Modern dentistry aims to preserve function, maintain oral health, and support a confident smile over the long term. Dental implants have become a central option because they replace the root as well as the visible crown, creating a foundation that integrates with bone through a process called osseointegration. This root-like stability can help distribute chewing forces efficiently and reduce the need to reshape neighboring teeth, a common requirement for traditional bridges. When a tooth is lost, bone in that area often resorbs; implant therapy can stimulate the jaw in a way that helps maintain volume and contour, which supports both function and facial aesthetics. For patients comparing alternatives, implants can complement conservative dentistry by offering a fixed solution that supports daily comfort and speech clarity.
To understand where implants fit, it helps to compare them with established approaches. A removable partial denture restores appearance and some function at a lower initial cost, but many patients notice movement during chewing and changes in taste or speech. A traditional bridge is fixed and can feel natural, yet it typically requires preparing adjacent teeth, which may be undesired if those teeth are healthy. An implant-supported crown replaces only the missing tooth and can be brushed and flossed similarly to a natural tooth space, which many people find convenient. Evidence from long-term studies reports high survival rates—often around or above nine in ten at ten years—when treatment is carefully planned and maintained.
The broader relevance within dentistry is preventive: missing teeth can lead to shifting, bite changes, and uneven wear that place stress on the temporomandibular joints. By restoring a stable chewing unit, implants can help maintain a balanced bite. They integrate well with other disciplines too. Periodontics supports healthy gums around the implant, endodontics may be considered for neighboring teeth, and prosthodontics customizes the crown or denture for function and appearance. In that sense, implant dentistry is not an isolated procedure but a team-based solution. For patients, the takeaway is practical—implants are one of the top options in a modern toolkit designed to protect oral health while prioritizing comfort, hygiene access, and durability.
Oral Surgery Pathway: From Evaluation to Implant Placement
Every successful implant begins with a thorough evaluation. Your clinician will review medical history, medications, and lifestyle factors such as tobacco use or bruxism, which can influence healing and long-term stability. Imaging—often including 3D scans—assesses bone height, width, and density while identifying nerves and sinus anatomy. This planning stage guides whether a graft is needed and what implant size and position will support the intended prosthetic outcome. A clear plan also clarifies the timeline, which may include immediate placement after extraction, early placement following soft-tissue healing, or delayed placement after complete site recovery.
On the day of surgery, anesthesia options are tailored to comfort and safety, ranging from local anesthesia to conscious sedation when appropriate. The key steps typically include a precise incision, gentle reflection of tissue, and a sequence of calibrated drills to create an osteotomy. The implant is placed to a planned depth and angulation, and primary stability is assessed. In many cases, a small healing abutment or cover screw is used, and the site is closed with fine sutures. Postoperative guidance focuses on protecting the area, managing discomfort, and maintaining hygiene with careful rinsing and targeted cleaning around the surgical site. Early healing for soft tissue often occurs within two weeks, while osseointegration progresses over several weeks to months, depending on bone quality and location.
Some patients benefit from adjunctive procedures. For the upper back jaw, a sinus lift may be recommended if the sinus floor is low; this elevates the membrane and adds graft material to create adequate height. For thin ridges, guided bone regeneration can widen the site using barrier membranes and bone substitutes. Where gum thickness is limited, connective tissue grafts may enhance soft-tissue contours. Not every case needs these additions, but discussing them helps set realistic expectations. Patients frequently ask about immediate teeth: provisional restorations can sometimes be delivered the same day, especially in cases with strong initial stability, but this is case-specific and balanced against the priority of uneventful healing.
Safety is an ongoing theme. Common-sense measures—such as controlling systemic conditions, coordinating with your physician on medications, and abstaining from smoking before and after surgery—can support healing. Practical tips include: – Use cold compresses intermittently for the first 24 hours; – Limit strenuous activity for several days; – Keep the surgical site clean without aggressive brushing; – Follow dietary guidance emphasizing soft, cool foods initially. With careful planning and adherence to postoperative instructions, most patients report steady progress through the early weeks and a smooth transition to the prosthetic phase.
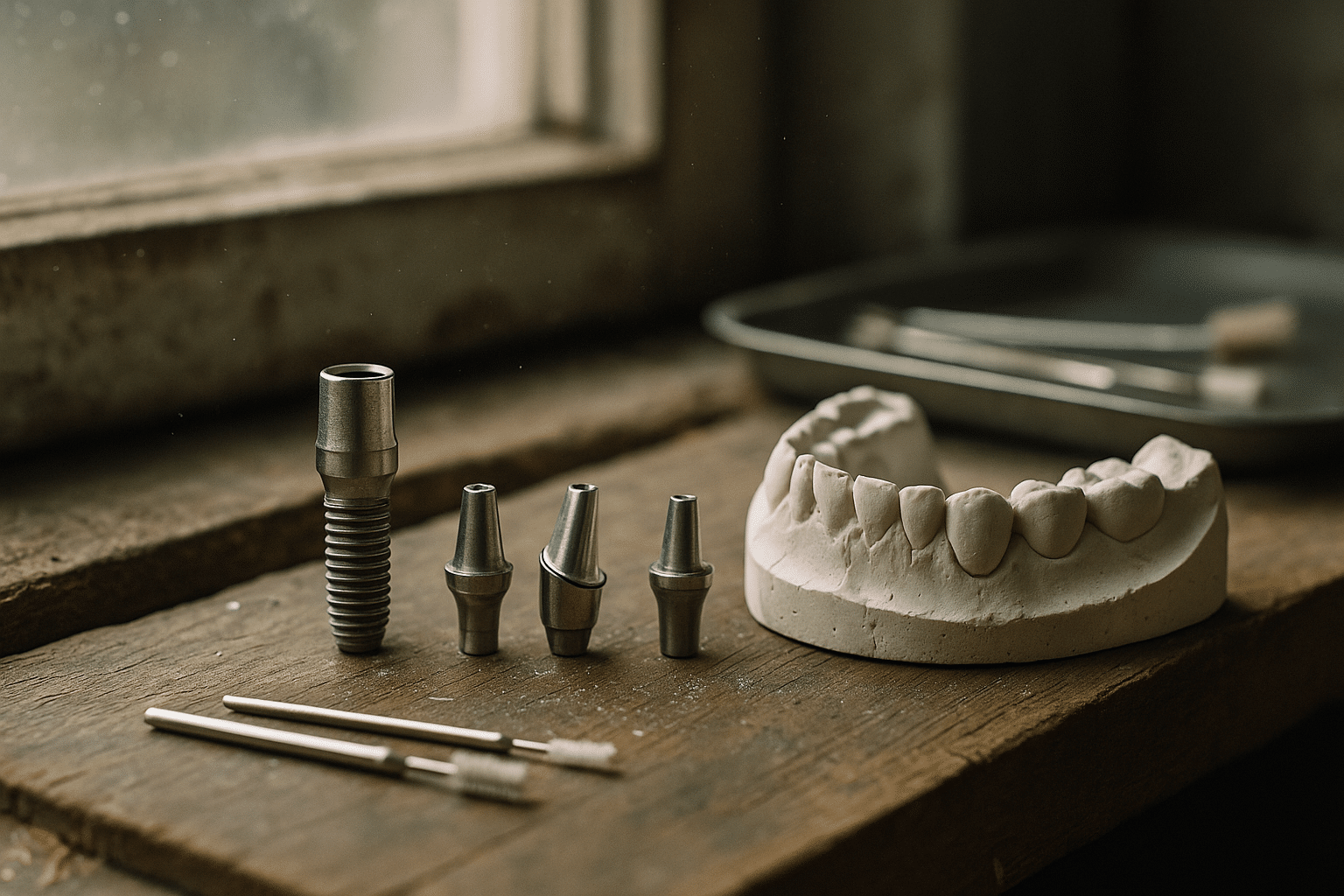
Prosthetic Options: Crowns, Bridges, and Implant-Supported Dentures
Once the implant integrates, the prosthetic phase brings the smile back into full function. For single-tooth replacement, an implant-supported crown is crafted to match the color and contour of surrounding teeth. The crown attaches via an abutment, either screwed into place or cemented. Screw-retained designs simplify retrievability for maintenance and avoid residual cement risk, while cement-retained crowns can offer refined esthetics by hiding the access channel. Material choices vary: ceramic systems can provide a lifelike appearance for front teeth, while layered combinations balance strength and translucency. Your clinician will weigh occlusal load, parafunctional habits, and location to select materials that align with function and appearance goals.
For multiple missing teeth in a row, an implant-supported bridge reduces the number of implants required while restoring a continuous chewing surface. Strategic positioning spreads forces and preserves hygiene access. Compared with a long traditional bridge, this approach avoids preparing adjacent natural teeth and can be easier to clean with tools like interdental brushes and water flossers. For patients missing all or most teeth, full-arch solutions provide a spectrum from removable overdentures that snap onto implants to fixed hybrid prostheses that stay in place. Overdentures use attachments—such as dome-shaped or bar-supported components—to enhance retention while remaining removable for cleaning. Fixed options are anchored with multiple implants and can feel very stable for chewing and speech.
Choosing among these paths involves balancing comfort, maintenance, and budget. Factors to discuss include: – Daily cleaning routines you are comfortable performing; – Desire for a removable versus fixed experience; – Tolerance for periodic screw checks and professional maintenance; – Priorities for speech clarity and chewing efficiency. Many patients value the simplicity of a fixed solution, while others prefer the flexibility of a removable prosthesis they can clean outside the mouth. The good news is that modern prosthodontics offers modularity: you can start with a removable design and later convert to a fixed option in some cases, depending on implant positions and bone support.
The final fitting is both technical and artistic. Clinicians verify the bite, refine contact points, and confirm that the prosthesis distributes forces evenly. Attention to tissue contours supports easy hygiene, helping you reach under bridges or along the gumline without frustration. Clear instructions, written and verbal, ensure you know how to care for the new restoration from day one. When prosthetics align with biology and patient preferences, the result is a durable, natural-feeling part of your daily life.
Longevity, Risks, and Maintenance: What Evidence Shows
Implant therapy is widely reported to perform reliably over many years when supported by sound planning and attentive maintenance. Published data often cite survival rates around or above 90% at ten years, though outcomes vary with factors like bone quality, systemic health, and oral hygiene. Complications can occur, and understanding them helps you prevent problems early. The two most discussed biological issues are peri-implant mucositis (inflammation confined to the soft tissue) and peri-implantitis (inflammation with bone loss). Mechanical concerns include screw loosening, veneer chipping, or wear of attachment components in overdentures. None of these are inevitable, and most are manageable with routine care and periodic checks.
Home care routines are the quiet heroes of longevity. Effective daily habits typically include: – Brushing twice daily around implants and gums; – Using interdental brushes sized to fit under bridges or around abutments; – Cleaning under fixed full-arch prostheses with super floss or water flossers; – Wearing a nightguard if you grind your teeth; – Limiting tobacco use and managing dry mouth. Professional maintenance visits allow for monitoring tissue health, removing calcified deposits, and checking torque values and occlusion. The interval is personalized—some patients do well on six-month recalls, while others benefit from visits every three to four months, especially in the first year.
Risk assessment is equally practical. People with uncontrolled diabetes, heavy smoking habits, or active periodontal disease have higher complication rates; addressing these factors first can improve outcomes. Bite forces matter too—patients with strong clenching or grinding may require occlusal guards and robust materials. For full-arch prostheses, evenly distributing implants and optimizing design reduces stress on the framework and attachments. If a complication arises, early communication helps. A small chip in a veneer, minor tissue irritation, or a loosened screw often has a straightforward fix when addressed promptly.
How do implants compare with other solutions over time? Traditional bridges can serve reliably, especially when adjacent teeth need crowns anyway, but if a supporting tooth fails, the entire bridge is affected. Removable dentures are cost-effective and quick to deliver but may require relines as the bone changes. Implants can help maintain bone volume by transmitting functional load to the jaw, supporting facial structure and chewing efficiency. Ultimately, the most suitable path respects your health profile, preferences, and maintenance commitment, with a care plan that evolves as your needs change.
Conclusion and Next Steps: Making a Confident, Informed Choice
Dental implants bring together surgical precision and prosthetic customization to restore function in a way that feels natural day to day. They are well-regarded for stability, hygiene access, and long-term performance when planned thoughtfully and maintained consistently. If you are exploring options, start with a comprehensive examination and candid conversation about your health history, expectations, and budget. Ask your clinician to map the journey from assessment to final prosthesis, including any grafting, provisional steps, and the timeline for integration and fitting. Clear planning reduces surprises and helps you participate fully in decisions that affect your comfort and lifestyle.
Consider preparing a short checklist for your consultation: – What imaging will be used, and what does it reveal about bone quantity and quality? – Are grafts or sinus procedures advisable, and why? – Which prosthetic design aligns with my cleaning habits and speech priorities? – What maintenance schedule and protective devices (like a nightguard) are recommended? – What are the realistic milestones, from surgery to final teeth, and what contingencies exist? These questions encourage transparent dialogue and help your care team tailor a plan that matches your goals.
For many patients, the benefits extend beyond the mirror. A secure bite can support a varied diet, reduce stress on remaining teeth, and contribute to jaw comfort. The journey does require patience—healing and customization take time—but the payoff is a restoration designed to serve your daily life with dependable function. If you value evidence-based care and want a solution that respects both biology and design, dental implants are among the most compelling options to discuss. With a thoughtful plan and steady maintenance, you can move forward confidently toward a stable, comfortable, and attractive smile.